- What is appendicitis?
- What is the appendix?
- What causes appendicitis?
- Who gets appendicitis?
- What are the symptoms of appendicitis?
- How is appendicitis diagnosed?
- How is appendicitis treated?
- What are the complications and treatment of a burst appendix?
- What if the surgeon finds a normal appendix?
- Can appendicitis be treated without surgery?
- What should people do if they think they have appendicitis?
- Eating, Diet, and Nutrition
- Points to Remember
- Hope through Research
- For More Information
What is appendicitis?
Appendicitis is inflammation of the appendix. Appendicitis is the leading cause of emergency abdominal operations.
1
1Spirt MJ. Complicated intra-abdominal infections: a focus on appendicitis and diverticulitis.
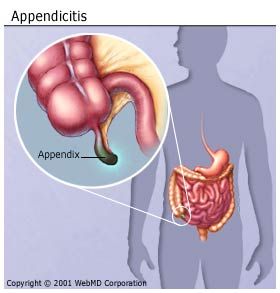
What is the appendix?
The appendix is a fingerlike pouch attached to the large intestine in
the lower right area of the abdomen, the area between the chest and
hips. The large intestine is part of the body’s gastrointestinal (GI)
tract. The GI tract is a series of hollow organs joined
in a long, twisting tube from the mouth to the anus. The movement of
muscles in the GI tract, along with the release of hormones and enzymes,
helps digest food. The appendix does not appear to have a specific
function in the body, and removing it does not seem to affect a person’s
health.
The inside of the appendix is called the appendiceal lumen. Normally,
mucus created by the appendix travels through the appendiceal lumen and
empties into the large intestine. The large intestine absorbs water from
stool and changes it from a liquid
to a solid form.
 The appendix is a fingerlike pouch attached to the large intestine in the lower right area of the abdomen.
The appendix is a fingerlike pouch attached to the large intestine in the lower right area of the abdomen.
What causes appendicitis?
An obstruction, or blockage, of the
appendiceal lumen causes appendicitis.
Mucus backs up in the appendiceal lumen,
causing bacteria that normally live inside
the appendix to multiply. As a result, the
appendix swells and becomes infected.
Sources of blockage include
- stool, parasites, or growths that clog the appendiceal lumen
- enlarged lymph tissue in the wall of the appendix, caused by infection in the
GI tract or elsewhere in the body
- inflammatory bowel disease (IBD), which includes Crohn’s disease
and ulcerative colitis, long-lasting disorders that cause irritation and
ulcers in the GI tract
- trauma to the abdomen
An inflamed appendix will likely burst if not removed.
Who gets appendicitis?
Anyone can get appendicitis, although it is more common among people 10 to 30 years old.
1
What are the symptoms of appendicitis?
The symptoms of appendicitis are typically easy for a health care
provider to diagnose. The most common symptom of appendicitis is
abdominal pain.
Abdominal pain with appendicitis usually
- occurs suddenly, often waking a person at night
- occurs before other symptoms
- begins near the belly button and then moves lower and to the right
- is unlike any pain felt before
- gets worse in a matter of hours
- gets worse when moving around, taking deep breaths, coughing, or sneezing
Other symptoms of appendicitis may include
- loss of appetite
- nausea
- vomiting
- constipation or diarrhea
- an inability to pass gas
- a low-grade fever that follows other symptoms
- abdominal swelling
- the feeling that passing stool will relieve discomfort
Symptoms vary and can mimic the following conditions that cause abdominal pain:
- intestinal obstruction—a partial or total blockage in the intestine that prevents the flow of fluids or solids.
- IBD.
- pelvic inflammatory disease—an infection of the female reproductive organs.
- abdominal adhesions—bands of tissue that form between abdominal
tissues and organs. Normally, internal tissues and organs have slippery
surfaces that let them shift easily as the body moves. Adhesions cause
tissues and organs to
stick together.
- constipation—a condition in which a person usually has fewer than
three bowel movements in a week. The bowel movements may be painful.
Appendicitis is an inflammation of the appendix,
a 3 1/2-inch-long tube of tissue that extends from the large intestine.
No one is absolutely certain what the function of the appendix is. One
thing we do know: We can live without it, without apparent consequences.
Appendicitis
is a medical emergency that requires prompt surgery to remove the
appendix. Left untreated, an inflamed appendix will eventually burst, or
perforate, spilling infectious materials into the abdominal cavity.
This can lead to
peritonitis,
a serious inflammation of the abdominal cavity's lining (the
peritoneum) that can be fatal unless it is treated quickly with strong
antibiotics.
Sometimes a pus-filled abscess
(infection that is walled off from the rest of the body) forms outside
the inflamed appendix. Scar tissue then "walls off" the appendix from
the rest of the
abdomen,
preventing infection from spreading. An abscessed appendix is a less
urgent situation, but unfortunately, it can't be identified without
surgery. For this reason, all cases of appendicitis are treated as
emergencies, requiring surgery.
In the U.S., one in
15 people will get appendicitis. Although it can strike at any age,
appendicitis is rare under age 2 and most common between ages 10 and 30.
What Are the Symptoms of Appendicitis?
The classic symptoms of appendicitis include:
- Dull pain near the navel or the upper abdomen that becomes sharp as it moves to the lower right abdomen. This is usually the first sign.
- Loss of appetite
- Nausea and/or vomiting soon after abdominal pain begins
- Abdominal swelling
- Fever of 99-102 degrees Fahrenheit
- Inability to pass gas
Almost half the time, other symptoms of appendicitis appear, including:
- Dull or sharp pain anywhere in the upper or lower abdomen, back, or rectum
- Painful urination
- Vomiting that precedes the abdominal pain
- Severe cramps
- Constipation or diarrhea with gas
If
you have any of the mentioned symptoms, seek medical attention
immediately since timely diagnosis and treatment is very important. Do
not eat, drink, or use any pain remedies, antacids, laxatives, or heating pads, which can cause an inflamed appendix to rupture.
How is appendicitis diagnosed?
A health care provider can diagnose most cases of appendicitis by taking a person’s medical history and performing a physical
exam.
If a person does not have the usual symptoms, health care
providers may use laboratory and imaging tests to confirm appendicitis.
These tests also may help diagnose appendicitis in people who cannot
adequately describe their symptoms, such as children or people who are
mentally
impaired.
Medical History
The health care provider will ask specific questions about
symptoms and health history. Answers to these questions will help rule
out other conditions. The health care
provider will want to know
- when the abdominal pain began
- the exact location and severity of the pain
- when other symptoms appeared
- other medical conditions, previous illnesses, and surgical procedures
- whether the person uses medications, alcohol, or illegal drugs
Physical Exam
Details about the person’s abdominal pain are key to diagnosing
appendicitis. The health care provider will assess the pain by touching
or applying pressure to specific areas of the abdomen.
Responses that may indicate appendicitis include
-
Rovsing’s sign. A health care provider
tests for Rovsing’s sign by applying hand pressure to the lower left
side of the abdomen. Pain felt on the lower right side of the abdomen
upon the release of pressure on the left side indicates the presence of
Rovsing’s sign.
-
Psoas sign. The right psoas muscle runs
over the pelvis near the appendix. Flexing this muscle will cause
abdominal pain if the appendix is inflamed. A health care provider can
check for the psoas sign by applying resistance to the right knee as the
patient tries to lift the right thigh while lying down.
-
Obturator sign. The right obturator muscle
also runs near the appendix. A health care provider tests for the
obturator sign by asking the patient to lie down with the right leg bent
at the knee. Moving the bent knee left and right requires flexing the
obturator muscle and will cause abdominal pain if the appendix is
inflamed.
-
Guarding. Guarding occurs when
a person subconsciously tenses the abdominal muscles during an exam.
Voluntary guarding occurs the moment the health care provider’s hand
touches the abdomen. Involuntary guarding occurs before the health care
provider actually makes contact and is a sign the appendix is inflamed.
- Rebound tenderness. A health care provider
tests for rebound tenderness by applying hand pressure to a person’s
lower right abdomen and then letting go. Pain felt upon the release of
the pressure indicates rebound tenderness and is a sign the appendix is
inflamed. A person may also experience rebound tenderness as pain when
the abdomen is jarred—for example, when a person bumps into something or
goes over a bump in a car.
Women of childbearing age may be asked to undergo a pelvic exam
to rule out gynecological conditions, which sometimes cause abdominal
pain similar to appendicitis.
The health care provider also may examine the rectum, which can be tender from appendicitis.
Laboratory Tests
Laboratory tests can help confirm the diagnosis of appendicitis or find other causes of abdominal pain.
-
Blood tests. A blood test involves drawing a
person’s blood at a health care provider’s office or a commercial
facility and sending the sample to a laboratory for analysis. Blood
tests can show signs of infection, such as a high white blood cell
count. Blood tests also may show dehydration or fluid and electrolyte
imbalances. Electrolytes are chemicals in the body fluids, including
sodium, potassium, magnesium, and chloride.
- Urinalysis. Urinalysis is testing of a urine
sample. The urine sample is collected in a special container in a health
care provider’s office, a commercial facility, or a hospital and can be
tested in the same location or sent to a laboratory for analysis.
Urinalysis is used to rule out a urinary tract infection or a kidney
stone.
- Pregnancy test. Health care providers also may order a pregnancy test for women, which can be done through a blood or urine test.
Imaging Tests
Imaging tests can confirm the diagnosis of appendicitis or find other causes of abdominal pain.
- Abdominal ultrasound. Ultrasound uses a
device, called a transducer, that bounces safe, painless sound waves off
organs to create an image of their structure. The transducer can be
moved to different angles to make it possible to examine different
organs. In abdominal ultrasound, the health care provider applies gel to
the patient’s abdomen and moves a hand-held transducer over the skin.
The gel allows the transducer to glide easily, and it improves the
transmission of the
signals. The procedure is performed in a health care provider’s office,
an outpatient center, or a hospital by a specially trained technician,
and the images are interpreted by a radiologist—a doctor who specializes
in medical imaging; anesthesia is not
needed. Abdominal ultrasound creates images of the appendix and can show
signs of inflammation, a burst appendix, a blockage in the appendiceal
lumen, and other sources of abdominal pain. Ultrasound is the first
imaging test
performed for suspected appendicitis in infants, children, young adults,
and pregnant women.
- Magnetic resonance imaging (MRI). MRI
machines use radio waves and magnets to produce detailed pictures of the
body’s internal organs and soft tissues without using x rays. The
procedure is performed in an outpatient center or a hospital by a
specially
trained technician, and the images are interpreted by a radiologist.
Anesthesia is not needed, though children and people with a fear of
confined spaces
may receive light sedation, taken by mouth. An MRI may include the
injection of special dye, called contrast medium. With most MRI
machines,
the person lies on a table that slides into a tunnel-shaped device that
may be open ended or closed at one end; some machines are designed to
allow the person to lie in a more open space. An
MRI can show signs of inflammation, a burst appendix, a blockage in the
appendiceal lumen, and other sources of abdominal pain. An MRI used to
diagnose appendicitis and other sources of abdominal pain is a safe,
reliable alternative to a computerized tomography (CT) scan.2
- CT scan. CT scans use a combination of x rays
and computer technology to create three-dimensional (3-D) images. For a
CT scan, the person may be given a solution to drink and an injection
of contrast medium. CT scans require the person to lie on a table that
slides into
a tunnel-shaped device where the x rays are taken. The procedure
is performed in an outpatient center or a hospital by an x-ray
technician, and the images are interpreted by a radiologist; anesthesia
is not needed. Children may be given a sedative to help them
fall asleep for the test. A CT scan of the abdomen
can show signs of inflammation, such as an enlarged appendix or
an abscess—a pus-filled mass that results from the body’s attempt to
keep an
infection from spreading—and other sources of abdominal pain,
such as
a burst appendix and a blockage in the appendiceal lumen. Women
of childbearing age should have a pregnancy test before undergoing
a CT scan. The radiation used in CT scans can be harmful to a
developing fetus.
2Heverhagen J, Pfestroff K,
Heverhagen A, Klose K, Kessler K, Sitter H. Diagnostic accuracy of
magnetic resonance imaging: a prospective evaluation of patients with
suspected appendicitis (diamond).
Journal of Magnetic Resonance Imaging. 2012;35:617–623.
How is appendicitis treated?
Appendicitis is typically treated with surgery to remove the
appendix. The surgery is performed in a hospital; general anesthesia is
needed. If appendicitis is suspected, especially in patients who have
persistent abdominal pain and fever, or signs of a burst appendix and
infection, a health care
provider will often suggest surgery without conducting diagnostic
testing. Prompt surgery decreases the chance that the
appendix will burst.
Surgery to remove the appendix is called an appendectomy. A surgeon performs the surgery using one of the following methods:
- Laparotomy. Laparotomy removes the
appendix through a single incision in the lower right area of the abdomen.
- Laparoscopic surgery. Laparoscopic surgery uses several smaller incisions
and special surgical tools fed through the incisions to remove the appendix. Laparoscopic surgery leads to fewer
complications, such as hospital-related infections, and has a shorter recovery
time.
With adequate care, most people recover from appendicitis and do
not need to make changes to diet, exercise, or lifestyle. Surgeons
recommend limiting physical activity for the first 10 to 14 days after a
laparotomy and for the first 3 to 5 days after laparoscopic surgery.
What are the complications and treatment of a burst appendix?
A burst appendix spreads infection throughout the abdomen—a
potentially dangerous condition called peritonitis. A person with
peritonitis may be extremely ill and have nausea, vomiting, fever, and
severe abdominal tenderness. This condition requires immediate surgery
through laparotomy to clean the abdominal cavity and remove the
appendix. Without prompt treatment, peritonitis can cause death.
Sometimes an abscess forms around a burst appendix—called an
appendiceal abscess. A surgeon may drain the pus from the abscess during
surgery or, more commonly, before surgery. To drain an abscess, a tube
is placed in the abscess through the abdominal wall. The drainage tube
is left in place for about 2 weeks while antibiotics are given to treat
infection. Six to 8 weeks later, when infection and inflammation are
under control, surgeons operate to remove what remains of the burst
appendix.
What if the surgeon finds a normal appendix?
Occasionally, a surgeon finds a normal
appendix. In this case, many surgeons will
remove it to eliminate the future possibility
of appendicitis. Occasionally, surgeons
find a different problem, which may also be
corrected during surgery.
Can appendicitis be treated without surgery?
Nonsurgical treatment may be used if surgery is not available, a
person is not well enough to undergo surgery, or the diagnosis is
unclear. Nonsurgical treatment includes antibiotics to treat infection.
What should people do if they think they have appendicitis?
Appendicitis is a medical emergency that requires immediate
care. People who think they have appendicitis should see a health care
provider or go to the emergency room right away. Swift diagnosis and
treatment reduce the chances the appendix will burst and improve
recovery time.
Eating, Diet, and Nutrition
Researchers have not found that eating,
diet, and nutrition play a role in causing or
preventing appendicitis. If a health care
provider prescribes nonsurgical treatment for
a person with appendicitis, the person will be
asked to follow a liquid or soft diet until the
infection subsides. A soft diet is low in fiber
and is easily digested in the GI tract. A soft
diet includes foods such as milk, fruit juices,
eggs, puddings, strained soups, rice, ground
meats, fish, and mashed, boiled, or baked
potatoes. People can talk with their health
care provider to discuss dietary changes.
Points to Remember
- Appendicitis is inflammation of the
appendix.
- The appendix is a fingerlike pouch
attached to the large intestine and
located in the lower right area of the
abdomen. The inside of the appendix is
called the appendiceal lumen.
- An obstruction, or blockage, of the appendiceal lumen causes appendicitis.
- The most common symptom of
appendicitis is abdominal pain. Other
symptoms of appendicitis may include
loss of appetite, nausea, vomiting,
constipation, diarrhea, an inability to
pass gas, a low-grade fever, abdominal
swelling, and the feeling that passing
stool will relieve discomfort
- A health care provider can diagnose
most cases of appendicitis by taking a
person’s medical history and performing
a physical exam. If a person does not
have the usual symptoms, health care
providers may use laboratory and
imaging tests to confirm appendicitis.
- Appendicitis is typically treated with surgery to remove the appendix.
- Nonsurgical treatment may be used
if surgery is not available, a person is
not well enough to undergo surgery, or
the diagnosis is unclear. Nonsurgical
treatment includes antibiotics to treat
infection.
- Appendicitis is a medical emergency that requires immediate care.
- If a health care provider prescribes nonsurgical treatment
for a person with appendicitis, the person will be asked to follow a
liquid or soft diet until the infection subsides.
Hope through Research
The National Institute of Diabetes and
Digestive and Kidney Diseases (NIDDK)
and other components of the National
Institutes of Health (NIH) conduct and
support basic and clinical research into many
digestive disorders, including appendicitis.
Clinical trials are research studies involving
people. Clinical trials look at safe and
effective new ways to prevent, detect, or
treat disease. Researchers also use clinical
trials to look at other aspects of care, such
as improving the quality of life for people
with chronic illnesses. To learn more about
clinical trials, why they matter, and how to
participate, visit the NIH Clinical Research
Trials and You website at
www.nih.gov/health/
clinicaltrials. For information about current
studies, visit
www.ClinicalTrials.gov.
For More Information
American Academy of Family Physicians
P.O. Box 11210
Shawnee Mission, KS 66207–1210
Phone: 1–800–274–2237 or 913–906–6000
Email:
contactcenter@aafp.org
Internet:
www.aafp.org American College of Surgeons
American College of Surgeons
633 North Saint Clair Street
Chicago, IL 60611–3211
Phone: 1–800–621–4111 or 312–202–5000
Fax: 312–202–5001
Email:
postmaster@facs.org
Internet:
www.facs.org American Society of Colon and Rectal Surgeons
American Society of Colon and Rectal Surgeons
85 West Algonquin Road, Suite 550
Arlington Heights, IL 60005
Phone: 847–290–9184
Fax: 847–290–9203
Email:
ascrs@fascrs.org
Internet:
www.fascrs.org
how to sell a diamond